The post Frequent Urination During Pregnancy and What You Can Do About It appeared first on Prenate Vitamin Family.
]]> Are you pregnant and finding yourself getting familiar with the inside of the ladies’ room? Frequent urination is common during pregnancy, especially for first-time moms. Learn more about the causes of frequent urination and what you can do to manage it.
Are you pregnant and finding yourself getting familiar with the inside of the ladies’ room? Frequent urination is common during pregnancy, especially for first-time moms. Learn more about the causes of frequent urination and what you can do to manage it.
Causes of Frequent Urination During Pregnancy
Thanks to the increased levels of the pregnancy hormone HCG and progesterone, the blood flow to your kidneys increases during pregnancy, causing you to visit the bathroom more frequently. While you might start seeing this common symptom as early as the first couple of weeks after conception, most women experience the urgency to urinate starting at week 10. That’s when the uterus begins putting pressure on the bladder.1
Symptoms of Frequent Urination
Frequent urination can be one of the first signs of pregnancy, and the urgency can increase during the first trimester. In addition to the frequency, leakage – also called stress urinary incontinence (SUI) – can occur during certain events, including2:
- sneezing
- coughing
- laughing
- exercising
- lifting
- walking
How to Manage Frequent Urination
Want to gain control over your frequent flow? Here are some suggestions.
Practice Kegel exercises. These exercises can strengthen the muscles of the pelvis and urethra and support the bladder. Kegel exercises are performed by first relaxing the abdomen, chest, thighs, and bottom. Next, contract the pelvic floor and hold for 5 seconds to 10 seconds. Relax the muscles for 5 to 10 seconds, then repeat the exercises 10 times.
Empty your bladder completely. Each time you go to the bathroom, lean forward as you urinate.
Cut back on fluids before bed. This will keep you from getting up in the middle of the night.
Avoid caffeine. Caffeine is a diuretic, and it will cause you to have to urinate more frequently.
While it may be tempting to skimp on fluids during the day to help reduce trips to the bathroom, don’t! Staying hydrated during pregnancy is extremely important. You should drink eight to 12 cups of water a day.3
Prenate® Vitamin Family
This post is brought to you by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.
The post Frequent Urination During Pregnancy and What You Can Do About It appeared first on Prenate Vitamin Family.
]]>The post The Biggest Pregnancy Myths: Debunked appeared first on Prenate Vitamin Family.
]]> You’ve probably heard them all – “pregnant women need to eat twice as much” and “having sex while pregnant can hurt the baby.” You may be wondering if any of the advice you’ve heard is true. We’ve compiled a list of common pregnancy myths that doctors have debunked.
You’ve probably heard them all – “pregnant women need to eat twice as much” and “having sex while pregnant can hurt the baby.” You may be wondering if any of the advice you’ve heard is true. We’ve compiled a list of common pregnancy myths that doctors have debunked.
Myth 1: Pregnant women need to eat twice as much.
Reality: Generally, moms-to-be only need 200 calories a day more than what’s required for a traditional healthy diet. The actual extra number of calories you need will depend on your normal weight and height, and activity level. The additional calories needed can easily be added with a healthy snack or two.
Myth 2: Pregnant women shouldn’t drink coffee.
Reality: You can drink coffee, but like everything else, while you’re pregnant, moderation is the key. Studies have proven that consuming more than two cups a day when pregnant could increase your chance of miscarriage.1
Myth 3: Pregnant women can have a glass of wine.
Reality: Consuming alcohol at any time during pregnancy isn’t safe. According to the U.S. Centers for Disease Control and Prevention (CDC), drinking alcohol in the first three months of pregnancy can cause a baby to have abnormal facial features.2
Myth 4: Cocoa butter prevents stretch marks.
Reality: There is no product – cocoa butter or otherwise – that can prevent stretch marks.
Stretch marks can be caused by both genetics and weight gain during pregnancy and may fade over time. It’s not recommended to spend money on products that promise to get rid of stretch marks.
Myth 5: Sex during pregnancy hurts the baby.
Reality: Sex does not have any effect on your growing baby. That little bundle of joy is protected by the tough muscles of the uterus and amniotic fluid. And the mucous plug blocks the opening of the cervix, protecting baby from any germs.3
Myth 6: How you carry your baby reveals the baby’s gender.
Reality: It’s a nice idea, but there is no proof that the shape of your belly can predict your baby’s gender. Whether you are carrying your baby low or high, it has no scientific bearing on gender.
Prenate® Vitamin Family
This post is brought to you by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.
The post The Biggest Pregnancy Myths: Debunked appeared first on Prenate Vitamin Family.
]]>The post Tips for Staying Hydrated While Pregnant appeared first on Prenate Vitamin Family.
]]> Dehydration is a serious concern for everyone during the hot summer months, but if you are expecting, you’re at a greater risk for complications such as neural tube defects, low amniotic fluid, inadequate breast milk production, and premature labor. Getting the right amount of water every day, and avoiding certain activities, will ensure you and baby-to-be remain hydrated.
Dehydration is a serious concern for everyone during the hot summer months, but if you are expecting, you’re at a greater risk for complications such as neural tube defects, low amniotic fluid, inadequate breast milk production, and premature labor. Getting the right amount of water every day, and avoiding certain activities, will ensure you and baby-to-be remain hydrated.
Recognizing Dehydration
When your body loses water faster than you can replenish it, and it struggles to keep up with its normal functions, that’s dehydration. Mild to moderate dehydration during pregnancy can cause a variety of symptoms, including:
- Dark yellow urine
- Dry, sticky mouth
- Lethargy
- Thirst
- Decreased need to urinate
- Headache
- Constipation
- Dizziness
Replacing lost water is crucial. But there are other things you can do to ensure that you and your baby-to-be are staying hydrated this summer while you’re pregnant. Here we share some valuable tips.
Drink Lots of Water
Water is the secret to staying hydrated. When you are expecting, water is even more crucial because it helps form amniotic fluid, produce extra blood, build new tissue, carry nutrients, enhance digestion, and flush out wastes and toxins. That’s a tall order, meaning you need more water than normal. The average person needs eight 8-ounce glasses a day, but moms-to-be should drink at least eight to 12 glasses a day.1
Increasing water intake can be a struggle, especially if you aren’t a fan of plain water. Here are few suggestions to make it easier:
- Infuse water with fruit or cucumbers.
- Swap out regular water for sparkling water.
- Set a timer to remind yourself to drink water throughout the day.
- Use an app that helps you track your water intake.
- Carry a reusable bottle with you when you are out and about.
- Drink a glass before every meal.
Eat More Foods High in Water Content
Water doesn’t have to come from a glass or a bottle. There are lots of fruits and vegetables that have high water content. Plus, they’re packed with vitamins and minerals, and antioxidants that are good for you and your little one-to-be! Here are some fruits and veggies to try2:
- Watermelon: 92% water
- Strawberries: 91% water
- Cantaloupe: 90% water
- Peaches: 89% water
- Celery: 95% water
- Cucumber: 95% water
- Lettuce: 96% water
Avoid Activities that Cause Overheating
If you are pregnant, you’re more likely to become overheated during the warmer seasons. That means you may want to put activities you used to enjoy pre-pregnancy on hold until after delivery. Here are some activities you should avoid:
- Exercising outdoors.
- Exercising in closed, hot rooms.
- Cooking in the kitchen on warm days.
- Soaking in hot tubs or relaxing in saunas.
Limit Time Spent Outside in Hot Climates
Getting outside in the warm summer months is tempting but can create unique risks to expecting moms. Pregnant women who have a body temperature above 102.2 degrees are at greater risk for heatstroke, heat exhaustion, and dehydration.3 Of course that doesn’t mean you can’t get outside and enjoy the weather – just limit your exposure and make sure you are well hydrated!
Prenate® Vitamin Family
This post is brought to you by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.
The post Tips for Staying Hydrated While Pregnant appeared first on Prenate Vitamin Family.
]]>The post What is hCG? Everything You Need to Know About the Pregnancy Hormone appeared first on Prenate Vitamin Family.
]]> Human chorionic gonadotropin, or hCG, is commonly referred to as the pregnancy hormone. It’s the hormone detected by home pregnancy tests and blood tests administered by your doctor. Although hCG levels can vary dramatically from pregnancy to pregnancy, most women’s bodies will produce the highest amount of hCG between seven and 12 weeks after a missed menstrual period.
Human chorionic gonadotropin, or hCG, is commonly referred to as the pregnancy hormone. It’s the hormone detected by home pregnancy tests and blood tests administered by your doctor. Although hCG levels can vary dramatically from pregnancy to pregnancy, most women’s bodies will produce the highest amount of hCG between seven and 12 weeks after a missed menstrual period.
Below you’ll find out everything you should know about hCG and what to discuss with your doctor if you have any concerns.
Different Women Have Different Levels
When you’re pregnant, it’s quite natural to compare notes with other expecting moms. But when it comes to hCG levels, comparing your levels with those of other pregnant women can cause needless worry. It’s not uncommon for one expecting mom to have much lower hCG levels than another woman, even if they are at the same point in their pregnancies.1
Differences in hCG levels can be caused by a variety of different factors, including how long it takes for an egg to get fertilized, travel down to the uterus, and implant itself into the uterine wall. As Heidi Murkoff, author of What to Expect When You’re Expecting puts it, “some embryos are simply zippier than others.”1
What is hCG?
hCG is a hormone that is produced once a woman becomes pregnant. The cells that eventually become the placenta begin to pump out hCG a few days after the embryo implants itself into the uterine wall.2 HCG helps ensure the corpus luteum (a temporary endocrine gland a woman’s body develops after ovulation) continues to produce progesterone during the first trimester of pregnancy.3
Should I Have My hCG Level Checked Often? What’s the Normal Level?
There really isn’t one exact number that represents a healthy hCG level for expecting moms. Because hCG levels can vary so much, it is not recommended that expecting mothers have their levels checked regularly. Instead, hCG levels should only be monitored if there are signs of a problem, such as cramping, bleeding, or a history of miscarriage.2
The hCG hormone is measured in milli-international units per milliliter (mIU/mL.) An hCG level above 25 mIU/mL indicates a positive pregnancy test. Any hCG level that is less than 5 mIU/ML indicates a negative pregnancy test. Levels that fall between 6 and 24 are a gray area and usually require retesting to confirm the results.
What if My hCG is High?
A higher level of hCG is not necessarily cause for concern. If your levels fall well outside of the typical range, it could be due to a few different factors. Most likely, it’s simply caused by a miscalculated due date. However, if your hCG level is extremely high, your doctor may also check for signs of molar pregnancy or multiple pregnancies.2
What if My hCG is Low?
A lower level of hCG doesn’t necessarily mean you should be concerned. Low hCG is often caused by a miscalculated due date. However, if your levels are extremely low, your doctor may check for signs of ectopic pregnancy or early miscarriage.2
Speak with a Doctor for More Information
Part of maintaining a healthy pregnancy is communicating openly with your healthcare provider. Be sure to ask them any questions you may have and discuss any concerns.
Prenate® Vitamin Family
This post is brought to you by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.

The post What is hCG? Everything You Need to Know About the Pregnancy Hormone appeared first on Prenate Vitamin Family.
]]>The post Rh Factor Blood Test & Pregnancy appeared first on Prenate Vitamin Family.
]]>
Sometimes, medical conditions that do not adversely affect a woman directly can have serious implications if she becomes pregnant. Rh blood type is one such factor in determining certain risks for pregnant women; therefore, your doctor will likely order an Rh blood screening during your first prenatal visit.1
What is Rh Factor and Why Does it Matter?
Rhesus (Rh) factor is an inherited protein found on the surface of red blood cells. If your blood contains the Rh factor, you are Rh positive. If your blood does not contain this protein, you are Rh negative. Rh positive is the most common blood type.1
Having an Rh negative blood type is not considered an illness and in most cases does not affect your health. However, if you are Rh negative and become pregnant, your pregnancy may require special care if your baby is Rh positive. This is known as Rh incompatibility.1
Rh Incompatibility During Pregnancy
Usually, the blood of mothers and their babies does not mix during pregnancy; however, sometimes blood can become intermingled during delivery or if the mother experiences bleeding or abdominal trauma during pregnancy. It may also occur during amniocentesis, chorionic villus sampling (CVS), or attempts to manually move the fetus out of breech position.1-2
If the blood of an Rh positive baby mixes with that of an Rh negative mother, the mother’s body will produce Rh antibodies after being exposed to the baby’s blood cells. It’s as if the mother’s body knows that the baby’s blood cells are not her own and her body produces these antibodies as a way of defending itself against what it interprets as an intruder.1-2
These antibodies are usually not a threat during pregnancy. However, they can lead to very serious problems in future pregnancies. If you are an Rh negative mother who produced antibodies during your first pregnancy, those antibodies can cross over the placenta during your next pregnancy and damage the red blood cells of your baby in utero. This can lead to a life-threatening form of anemia in which the baby’s red blood cells are destroyed faster than they can be replaced.1
Rh Blood Screening
The purpose of an Rh factor blood screening is to determine the mother’s Rh blood type early, preferably before or immediately after she becomes pregnant. If the mother’s blood screening shows that she is Rh negative, her doctor may advise her to take medication to prevent antibodies from forming.2
If you are Rh negative and there is a chance that your baby is Rh positive, your doctor may order an antibody screening. This is a separate blood test that determines if your body has already made antibodies in response to being exposed to Rh positive blood cells.2
Typically, Rh antibody screening is done during the first trimester and again at 28 weeks. In some cases, screenings may be done more frequently.2
Antibody Treatment
For women who have not been exposed to an incompatible Rh factor, their doctor may advise Rh immune globulin (RhIg) treatment once they become pregnant. RhIg is administered by injection, usually at 28 weeks of pregnancy and then again within 72 hours after the Rh-positive baby has been delivered.2
RhIg treatment is only effective if the woman has not already made Rh antibodies.1-2
If you are Rh negative and your body has already created antibodies in response to being exposed to Rh positive blood cells, your pregnancy may be considered higher risk. The development of the baby will be monitored very carefully, usually with ultrasound exams.2
If your baby develops severe anemia, early delivery (before 37 weeks) may be required. Alternatively, doctors may perform a blood transfusion through the umbilical cord while the baby is still inside your womb.2
If your baby’s anemia is mild, the delivery may occur at the normal time. However, the baby may require a blood transfusion after delivery.2
Prenate® Vitamin Family
This post is sponsored by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.
The post Rh Factor Blood Test & Pregnancy appeared first on Prenate Vitamin Family.
]]>The post Quarantine Exercises During Pregnancy appeared first on Prenate Vitamin Family.
]]> Staying active and committing to a regular exercise routine can help expecting mothers alleviate discomfort, strengthen muscles, and improve mood.1 Unfortunately, as the COVID-19 pandemic continues and stay-at-home orders remain in effect for much of the country, opportunities to exercise at our favorite workout venues are scarce. The good news is, despite quarantine restrictions, moms-to-be can stay active with a few simple, at-home workout routines.
Staying active and committing to a regular exercise routine can help expecting mothers alleviate discomfort, strengthen muscles, and improve mood.1 Unfortunately, as the COVID-19 pandemic continues and stay-at-home orders remain in effect for much of the country, opportunities to exercise at our favorite workout venues are scarce. The good news is, despite quarantine restrictions, moms-to-be can stay active with a few simple, at-home workout routines.
Always consult your physician before starting an exercise routine.
Pump & Kegel
The “pump and Kegel” exercise is quick and safe for most expecting mothers.
Here’s how to do it:
- Stand up straight with your hand over your abdomen.
- Inhale slowly, engaging your diaphragm, then release your core muscles.
- Next, use your abdominal muscles to hug the baby toward your body. (It helps to imagine zipping up a pair of pants that are a little too tight.) At the same time, do a Kegel exercise. A Kegel is when you give your pelvic floor muscles a gentle lift, contracting your pelvic muscles, holding them, and then releasing. (It helps to imagine you have to pee but are holding it in.)
- Repeat the process up to 20 times.
Here’s a quick video from The Bump to illustrate: https://youtu.be/GM7WrxZMWmc
At-Home Yoga
Yoga can be a great way for expecting moms to tune in to their changing bodies, improve flexibility and balance, reduce stress and anxiety, improve sleep, and more. For women who aren’t familiar with practicing yoga or need a little guidance, there are numerous free online videos and tutorials. YouTube is an excellent source of free information but always use common sense when following an online video. Is the person posting the video a qualified yoga instructor? Do they have real-life credentials? These are just a few things to keep in mind when following an online fitness or health “expert.”
If you want something a little more structured, there are multiple subscription-based online classes that instruct viewers on the practice of yoga, from beginners to masters. A few examples include omstars.com, glo.com, MyYogaWorks.com, and Gaia.com. Through these subscription-based websites, users can access information and online classes for a variety of different yoga styles and skill levels. The costs vary by website, but some offer a free trial period.
Total Body Workout
Don’t let the sound of “total body workout” intimidate you. These workouts might be a little more strenuous than doing yoga, but they can still be low-impact and done at your pace to ensure you don’t overdo it. Remember to rest as much as your body needs between circuits (one circuit is completing all exercises in the routine) and take frequent water breaks. Again, consult your doctor before beginning any prenatal workout routine.
Here’s an example circuit for a prenatal total body workout:
- Squat & Press – Stand with your feet hip-width apart. Hold a dumbbell in each hand at shoulder height for added resistance. Keeping your core engaged, lower yourself into a squat position with your rear end pushed back and your thighs as close to parallel to the ground as possible. Return to a standing position by pushing through your heels. If you added dumbbells, raise them over your head when you return to standing. Complete 15 reps.
- Quadruped Extension – Carefully get on your hands and knees, keeping your wrists aligned with your shoulders and your knees under your hips. Slowly extend your right leg to about hip-height behind you, then extend your left arm to shoulder height in front of you. Hold this position for a few seconds, then lower your arm and leg. Repeat using the opposite leg and arm to complete the rep. Do 15 reps.
- Side Plank & Leg Lift – Start in a modified side plank position, propping yourself up on your side with your left hand and your left knee on the ground and your left leg straight out behind you and touching the ground. Rest your right hand on your right hip. Engage your obliques as you lift and lower your right (top) leg for one rep. Do 12 reps, switch sides, and do 12 more.
- Complete the above circuit four days a week, two times a day, or at whatever frequency feels best for you.
Talk to Your Doctor
The exercises discussed in this post are likely safe for most expecting moms; however, you should always talk to your doctor before starting a prenatal exercise routine. Likewise, to maintain a fit and healthy lifestyle, you should incorporate good nutrition, emotional self-care, and regular medical checkups into your overall wellness plan. This will not only help you feel and look your best during pregnancy, but it also may provide benefits to your baby during gestation. Research indicates that women who exercise during pregnancy may be more likely to deliver closer to their due date and have a lower risk of developing gestational diabetes, while the babies themselves may exhibit better development in body composition, cardiovascular health, and nervous system development.2 Furthermore, research suggests that women who adopt a healthy lifestyle may be more likely to have a positive influence on their child’s postnatal health and decrease their child’s risk of developing chronic diseases such as obesity and diabetes.2
Prenate® Vitamin Family
This post is sponsored by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.

The post Quarantine Exercises During Pregnancy appeared first on Prenate Vitamin Family.
]]>The post Understanding Amniocentesis appeared first on Prenate Vitamin Family.
]]> Amniocentesis is a procedure that may help detect genetic abnormalities in babies before they are born. Although the process is considered safe, there are a few risks associated with amniocentesis. Expecting moms should educate themselves on the risks and benefits of amniocentesis and discuss the options with a healthcare provider.
Amniocentesis is a procedure that may help detect genetic abnormalities in babies before they are born. Although the process is considered safe, there are a few risks associated with amniocentesis. Expecting moms should educate themselves on the risks and benefits of amniocentesis and discuss the options with a healthcare provider.
What is Amniocentesis?
Amniocentesis is an invasive procedure in which a healthcare professional takes a sample of the amniotic fluid to test for chromosomal abnormalities, lung maturity, fetal infection, or paternity.1 The procedure is typically done after 15 weeks of gestation and if a mother’s triple test results show an abnormality. A triple test is a non-invasive blood test expecting mothers receive from a medical provider, usually between the 16th week and the 18th week of gestation, to screen for abnormal levels of AFP, hCG, and estriol.3
It is important to remember that the triple test does not diagnose any disorder, but rather screens for potential warning signs that indicate further testing should be done.3
How is Amniocentesis Performed?
Using ultrasound for guidance, a doctor will find a safe place to insert a needle to collect a sample of amniotic fluid (the fluid that surrounds a baby in the womb.) Although the entire process can sometimes take up to 45 minutes, the collection of amniotic fluid only takes about five minutes.1 Although moms may feel some pain during the process, it is generally well tolerated without any anesthesia.2
The amniotic fluid, which contains cells shed from the fetus, is then sent to the laboratory for analysis. The length of time it takes to get the results back can vary from a few days to a few weeks.1
Who Should Get an Amniocentesis?
Amniocentesis is not a required procedure for every expecting mother; however, your doctor may wish to perform an amniocentesis if any of the following statements apply to your situation:4
- You had abnormal results from a triple test or other prenatal screening tests. Amniocentesis can be used to confirm or rule out certain genetic disorders.
- You had chromosomal conditions or neural tube defects in a previous pregnancy.
- You are 35 or older. Babies born to women older than 35 have a higher risk of chromosomal conditions such as Down syndrome.
- You or the baby’s father is a known carrier of a genetic condition, or you have a family history of a specific genetic condition.
- Your ultrasound produced abnormal results.
- Early delivery is being considered to avoid pregnancy complications. Amniocentesis can be used to test a baby’s lung maturity, gauging whether he or she will be able to breathe effectively after early delivery.4
Weighing the Risks and Benefits
If any of the above statements apply to you, an amniocentesis may be highly beneficial in that it can ease anxiety or help you prepare for a baby who may have health or development complications. However, some expecting mothers may choose not to have an amniocentesis, even if the above indicators are present.
Reasons for opting not to have an amniocentesis can vary. Some expecting mothers feel comfortable going forward with a pregnancy regardless of any potential genetic problems; therefore, they don’t see the point in knowing about any problems ahead of time. On the other hand, some expecting mothers have moral, religious, or spiritual beliefs that would eliminate the option of terminating a pregnancy. Finally, some expecting mothers choose to avoid any tests or procedures that pose any risk to the baby. It is a very personal decision. While your doctor can make a recommendation on whether or not to get an amniocentesis, it is ultimately up to you.
The main risk associated with amniocentesis is miscarriage. Miscarriage can occur after amniocentesis due to infection in the uterus, water breaking, or labor being induced prematurely.1
According to the American Pregnancy Association, the risk of miscarriage associated with amniocentesis can range from 1 in 400 to 1 in 200.1 However, other sources report different findings. The AMA Journal of Ethics reports that risk of miscarriage within 14 days after the procedure was 0.6 percent; pregnancy loss before 24 weeks (the point at which a fetus is considered viable) was 0.9 percent; and pregnancy loss at any point following an amniocentesis was 1.9 percent. Authors of the study warned that these figures may underestimate the true added risk of invasive prenatal procedures.2
For expecting mothers who have an infection such as HIV or AIDS, hepatitis B, or hepatitis C, an amniocentesis may not be recommended, as the procedure could potentially pass the infection from the mother to the baby.4
Talk to Your Doctor
It’s normal to feel concerned about the risks of amniocentesis. Speak with your doctor to learn more about the procedure, including the potential risks and benefits. While amniocentesis can provide expecting mothers with peace of mind, it may not be right for everyone.
Prenate® Vitamin Family
This post is sponsored by the Prenate® Vitamin Family, a line of prescription prenatal supplements designed to enhance preconception, prenatal, and postpartum nutrition in women. Talk with your doctor about how taking a daily prescription prenatal or postnatal vitamin could help support a healthy pregnancy and postpartum wellness.
The post Understanding Amniocentesis appeared first on Prenate Vitamin Family.
]]>The post New Prenate® Direct Program Simplifies Your Prenatal Nutrition appeared first on Prenate Vitamin Family.
]]>
We’re excited to announce our new Prenate® Direct Program, designed to make getting your prenatal supplements more convenient than ever. We have partnered with GoGoMeds, an online pharmacy, to provide an easy and cost-effective way for patients to fill their prenatal vitamin prescriptions.
Life Doesn’t Wait
Whether you’re a first-time mom or the mother of many, you’ve got better things to do than wait in line at a pharmacy. Prenate® Direct and GoGoMeds let you fill your Prenate® prescription on your own time, from your home or on the go. Plus, our automatic refill option means you can fill your prescription less often and save more.
How It Works
Prenate® Direct and GoGoMeds offer a safe and secure way to fill pharmacy orders online and at a price you can afford. If you are new to Prenate® Direct and GoGoMeds, follow the steps below to set up your account and enter your prescription information.
Step 1 – Order
Ask your doctor to prescribe Prenate® by EMR, phone or fax.
- Phone: 888-481-3539
- Fax: 833-379-4402
- EMR: Search EMR for Specialty Medical Drugstore OR GoGoMeds, Southgate, KY 41071
- Pharmacy Type: MAIL or RETAIL
- NPI: 1659779064
- NCPDP: 1834793
Step 2 – Validate
Call GoGoMeds at 888-481-3539 to validate your address, contact information, insurance (or cash price if uninsured) and payment information.
Step 3 – Ship
Sit back while GoGoMeds mails your prescription directly to your home. Shipping is always free! So you just have to pay for the cost of your prescription.
Why GoGoMeds
GoGoMeds is owned and operated by Specialty Medical Drugstore, which is part of Fortis Holding Company. All GoGoMeds orders are filled out of the GoGoMeds’ headquarters in Southgate, Kentucky.
GoGoMeds is a Verified Internet Pharmacy Practice Site (VIPPS) accredited pharmacy. It is licensed to sell prescriptions in all 50 states and the District of Columbia. Click below to learn about GoGoMeds’ accreditations.
No Insurance? No Problem!
If you are uninsured or have insurance that does not cover prescription prenatal vitamins, Prenate® Direct is a perfect solution to help meet your prenatal needs. Filling your Prenate® prescription with Prenate® Direct and GoGoMeds guarantees you’ll get the lowest cash pricing for non-covered prescriptions.
Guaranteed Availability
Have you ever gone to the pharmacy with a prescription for a specific product but come home with a generic instead? Or has your Prenate® product been out of stock at times at your pharmacy? Our Prenate® Direct program ensures you get the right prescription every time. You can rest easy knowing that your prescription will be filled with the exact product your health care provider intended.
Optional Automatic Refills
With a 90-day prescription, patients have the option to have their Prenate® product refilled automatically. You don’t have to worry about calling before your prescription runs out. We’ll send it to you in advance to ensure you don’t miss a pill.
Looking for a Prescription Prenatal Vitamin?
Prenate® Vitamin Family offers a line of prescription nutritional supplements designed for all stages of pregnancy, from preconception through postpartum. Prenate® vitamins are formulated with the latest recommendations from obstetric and pediatric organizations in mind. Plus, nutrient forms are selected for their tolerability and absorbability. Talk with your doctor about whether a prescription prenatal vitamin from the Prenate® Vitamin Family may be right for you.

The post New Prenate® Direct Program Simplifies Your Prenatal Nutrition appeared first on Prenate Vitamin Family.
]]>The post Your Guide to the New Nutrition Labels appeared first on Prenate Vitamin Family.
]]>
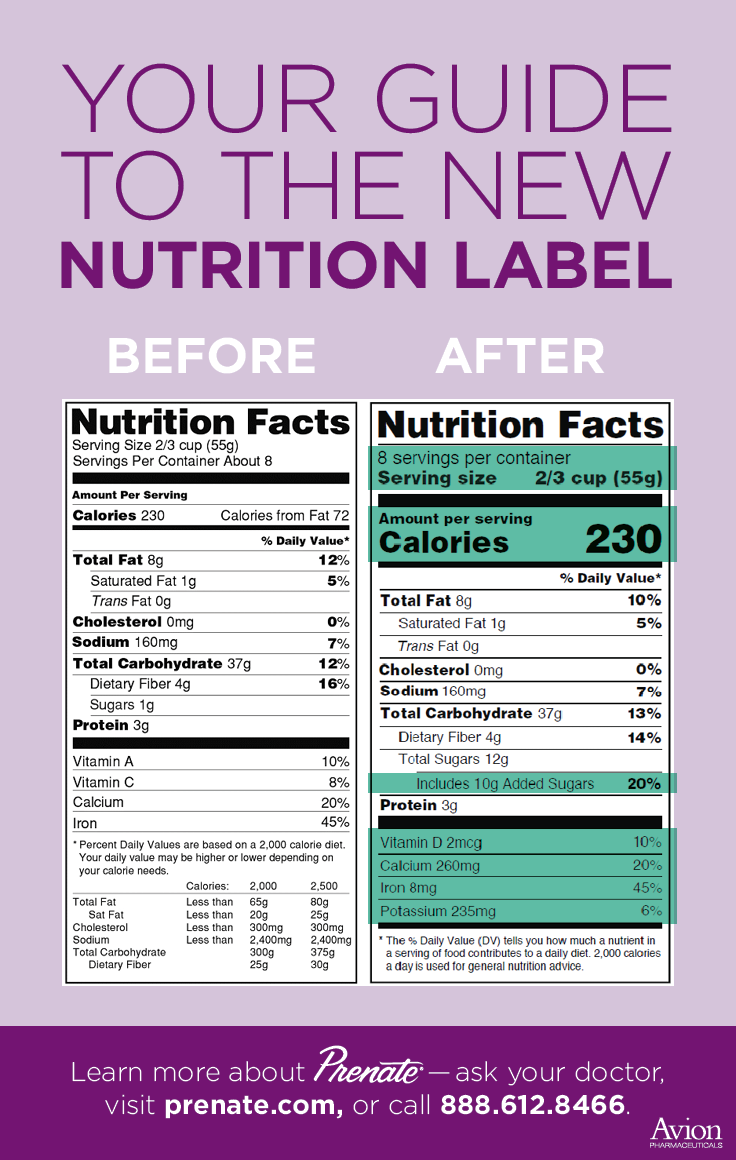
You may have noticed new nutrition labels on some of your favorite foods. Many manufacturers have already started including the new labels on their packaging. By May, a U.S. Food and Drug Administration (FDA) mandate will require most manufacturers to use the new nutrition label guidelines on product packaging.
As March is National Nutrition Month, it’s a good time to explain what information is included on the new labels. With an understanding of the new labels and the information they provide, expecting moms can make better and more informed food choices. While the overall look of the labels remains the same, there are some key updates that have big impacts.
Serving Sizes
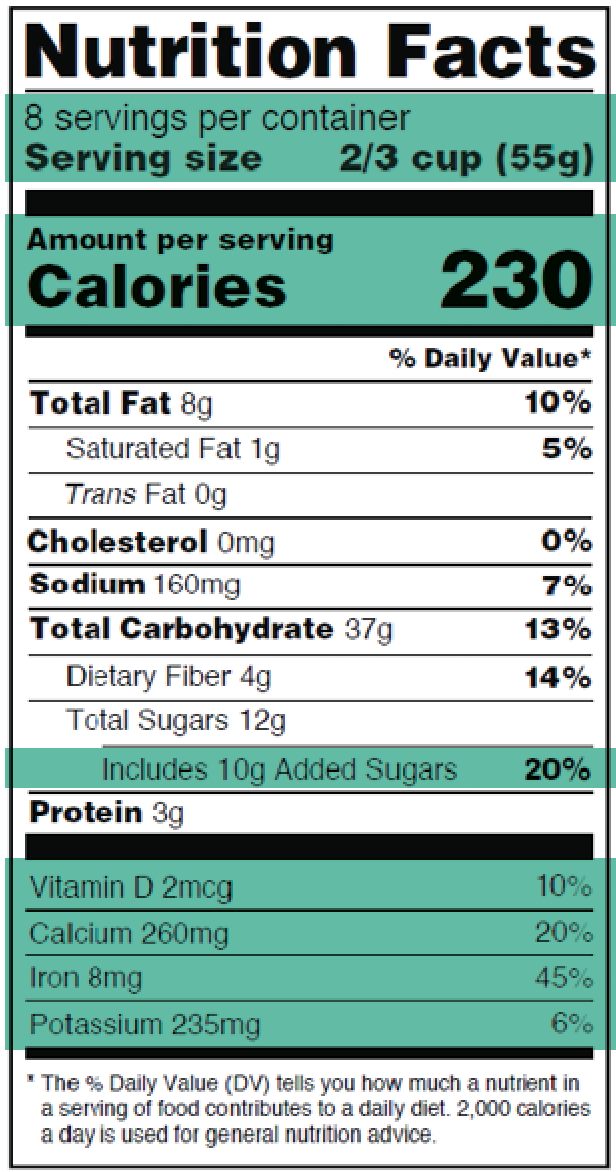 The total number of “servings per container” and “serving size” now use a larger font to make this information stand out more. In addition, the serving size values have been updated to reflect the eating and drinking habits of consumers today. In the past, you may have looked at a serving size and thought that it was far smaller than what you typically consumed. These values have been adjusted to reflect customary serving sizes. For example, a serving size for soda was previously 12 ounces. On the old label, a 20-once soda would be listed as 1.67 servings. However, most people would consume all the soda in a 20-ounce bottle in a single sitting. The new guidelines take packaging into consideration. So a 20-ounce bottle of soda is now a single serving on the new labels.
The total number of “servings per container” and “serving size” now use a larger font to make this information stand out more. In addition, the serving size values have been updated to reflect the eating and drinking habits of consumers today. In the past, you may have looked at a serving size and thought that it was far smaller than what you typically consumed. These values have been adjusted to reflect customary serving sizes. For example, a serving size for soda was previously 12 ounces. On the old label, a 20-once soda would be listed as 1.67 servings. However, most people would consume all the soda in a 20-ounce bottle in a single sitting. The new guidelines take packaging into consideration. So a 20-ounce bottle of soda is now a single serving on the new labels.
When making food choices it’s important to keep serving size in mind. Eating a single serving can help you better track the calories, nutrients, fat and sugars you consume. It can also help curb overeating. Cravings may happen during pregnancy, and being mindful of serving size can help you establish limits on foods you eat.
Calories
The “calories per serving” listing on the new labels is also much larger and bolder on the new nutrition labels. In addition, the “calories from fat” has been removed from the new labels. Research has shown that the type of fat is more important than the number of calories from fat.1
When making food choices, expecting moms should try to keep track of the calories they consume. Maintaining a healthy weight is important for positive pregnancy outcomes. The new nutrition label features an updated footnote that indicates that daily values are based on a 2,000-calories-a-day diet. Your health care provider can discuss ideal ranges for daily calorie consumption. But the new nutrition labels highlight this information to help people make informed decisions.
Daily Values
The daily value percentages have been adjusted to reflect new scientific evidence. As a general rule, a daily value of below 5 percent is considered low and above 20 percent is considered high. For example, a food that has a sodium daily value of 25 percent is considered high. Or a food that contains 30 percent daily value of calcium would be considered high in calcium. As with calories, you do not want to overly exceed daily value recommendations, particularly with fats, sugars or sodium.
Required Nutrient Information
Manufacturers must now include the amount and daily percent value of vitamin D, calcium, iron and potassium. Research has shown that many Americans do not regularly consume enough of these nutrients.1 By including them on the labels, the FDA hopes to highlight their importance in a well-balanced diet. Similarly, vitamin A and vitamin C have been removed as required nutrients. Research has shown that deficiencies in these nutrients are rare.1
The new nutrition labels now include added sugars. Expecting moms want to have less than 10 percent of their calories from added sugars. These are empty calories that do not have nutritional value.
Pregnancy Nutrition
Generally speaking, women should aim to eat less saturated fat, trans fat, sodium and added sugars. To improve positive health and pregnancy outcomes, aim for less than 100 percent daily value on these nutrients. When making food choices, aim for more fiber, vitamin D, calcium, iron, potassium and especially folate during preconception and early pregnancy. Many Americans do not get enough of these critical nutrients.
To fill nutritional gaps and ensure that their babies receive sufficient vitamins and minerals, expecting moms should take a daily prenatal vitamin. The Prenate® Vitamin Family offers a line of prenatal vitamins that are designed to carry moms and their babies through preconception to pregnancy and into the weeks and months after delivery.
All Prenate® vitamins contain 1 mg of folate and many contain iron, calcium and vitamin D. The nutrient forms were selected because they are essential for maintaining a healthy pregnancy diet. You can find a comparison of nutrients in each Prenate® by clicking the link below. Talk to your doctor to see if a Prenate® vitamin is right for you.
Prenate Nutrient Comparisons:
https://prenate.com/the-prenate-family/prenate-productcomparison/
The post Your Guide to the New Nutrition Labels appeared first on Prenate Vitamin Family.
]]>The post The Importance of Your Relationship with Your Health Care Provider During Pregnancy appeared first on Prenate Vitamin Family.
]]>
Prescription prenatal vitamins are important for both mothers and their babies. Prenatal vitamins are a critical factor in maintaining a healthy pregnancy, but not all prenatal vitamins are the same. Women deserve to choose the option that is right for them. Health care experts can play an important role in helping women determine which prenatal vitamin meets their needs. However, a proposed change to how vitamins are categorized may take health care providers out of the decision-making process, and this could have a devastating effect for women who are pregnant or trying to conceive.
Take Action to Protect Your Right to Rx Prenatal Vitamins
Send Email Tweet @FDB_US Send a Letter
Trusted Relationship with Health Care Provider
Every pregnancy is unique, and each expecting mother should be given specific nutritional recommendations, as determined by a prescriber evaluation. Prescription prenatal vitamins enable health care providers to deliver the gold standard of prenatal nutritional support to their patients.
For more than 35 years, health care providers have prescribed Prenate® Vitamin Family products to their patients. Both patients and health care providers have relied on these and other prescription vitamins to help reduce the risks of birth defects and other negative pregnancy outcomes. With quality assurance and optimal nutrient levels, Prenate® and other prescription prenatal vitamins support the health and well-being of mothers and babies.
By prescribing Prenate® or other prescription prenatal vitamins, health care providers can more closely mange the nutritional intake of their patients, with assurance that both moms and their babies are getting the nutrients they need.
Proposed Changes to the Standard of Prenatal Nutritional Care
According to reports, nearly 50 percent of pregnancies in the U.S. are unplanned, and only 11 percent of women ages 18 to 45 are aware that folic acid supplementation should begin before a woman tries to conceive.1-4 This lack of awareness is particularly troubling in light of a proposed change in the health care system that could have a major effect on the affordability and accessibility of prescription prenatal vitamins.
First Databank, Inc. is the primary publisher of pharmaceutical information that is used to negotiate insurance reimbursement rates paid to pharmacies and other providers. Currently, prescription prenatal supplements are categorized as a prescription product. First Databank is shifting policy to code all prescription prenatal vitamins into a class historically associated with over-the-counter products. This could immediately decrease women’s access to and choice about their prenatal vitamins – products that are universally regarded as crucial components of prenatal care. If the “over-the-counter” status goes into effect, there is the potential for prenatal nutritional decisions to fall mostly on the patient.
Speak Up to Protect the Health of Moms and Babies
With minimal public awareness of the importance of folic acid and the rate of unplanned pregnancies in the U.S., it is critical for health care and insurance providers to ensure that all patients have access to prescription prenatal vitamins.
Take action below to protect women’s rights to prescription prenatal vitamins.
Send Email Tweet @FDB_US Send a Letter
The post The Importance of Your Relationship with Your Health Care Provider During Pregnancy appeared first on Prenate Vitamin Family.
]]>

